How Dialysis Machines Work: A Step-by-Step Explanation
Dialysis machines are vital in supporting patients with chronic kidney failure or acute kidney injury, filtering blood to remove waste and excess fluid when kidneys cannot perform these functions effectively. Here, we’ll break down the working process of dialysis machines, providing a clear understanding of how these lifesaving devices work and their critical components.
1. Understanding the Purpose of Dialysis
Dialysis is required when kidney function falls below a threshold where the body can no longer remove waste and balance fluids independently. Patients undergoing dialysis often experience symptoms like swelling, fatigue, and difficulty breathing due to accumulated fluids and toxins. Dialysis machines help replace kidney function by removing these unwanted substances, stabilizing electrolyte levels, and managing fluid balance.
2. Types of Dialysis: Hemodialysis and Peritoneal Dialysis
- Hemodialysis: Blood is filtered outside the body using a dialysis machine.
- Peritoneal Dialysis: Blood is filtered inside the body using the peritoneum (a membrane in the abdomen).
While peritoneal dialysis uses a different setup, hemodialysis involves a machine to facilitate the filtration process. For this post, we’ll focus on hemodialysis machines.
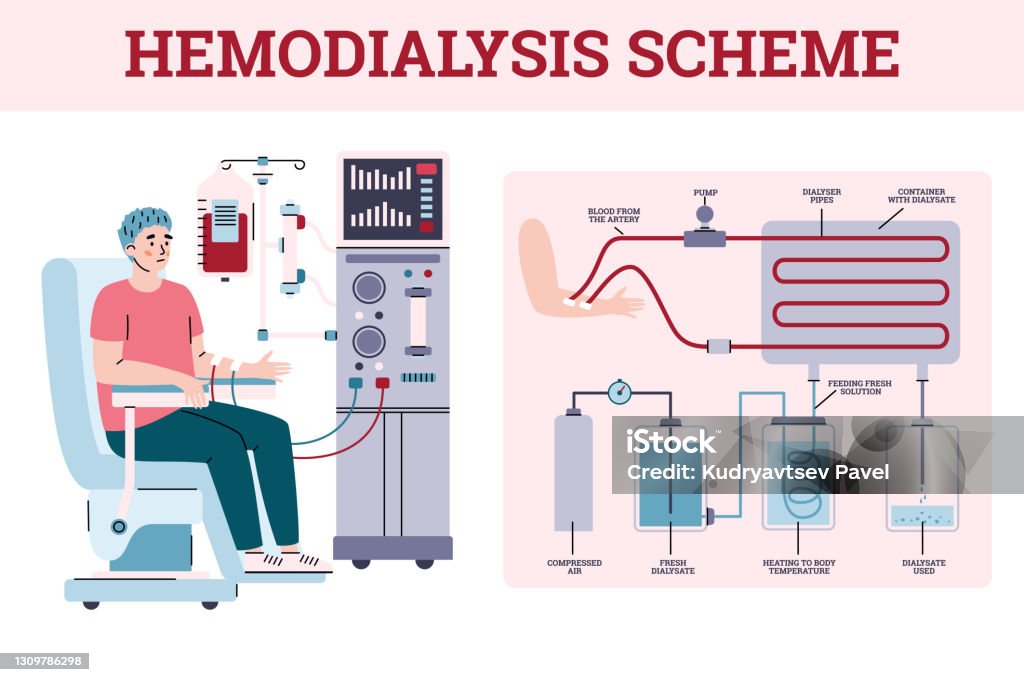
3. Key Components of a Hemodialysis Machine
- Dialyzer (Artificial Kidney): The core component, which filters the blood.
- Dialysate: A solution that absorbs waste from the blood, aiding filtration.
- Blood Pump: Moves blood from the patient to the machine and back.
- Monitoring System: Tracks blood pressure, flow, and other parameters.
- Heparin Pump: Prevents blood clotting during dialysis.
4. The Dialysis Process: Step-by-Step
Step 1: Blood Access
Access is achieved through a vascular access point—an arteriovenous (AV) fistula, graft, or catheter. This access is crucial for maintaining a high blood flow rate, essential for effective dialysis.
Step 2: Blood Pumping and Heparin Injection
Blood is drawn from the access point and sent through a blood pump. The pump regulates the flow rate, typically around 300-400 milliliters per minute, ensuring effective filtration. The heparin pump injects a small amount of heparin to prevent clotting as blood travels through the machine.
Step 3: Blood Filtration in the Dialyzer
The blood enters the dialyzer, where filtration occurs. The dialyzer consists of a semi-permeable membrane dividing it into two chambers—one for blood and the other for dialysate. Blood flows on one side of the membrane, while dialysate flows on the opposite side. The concentration difference between blood and dialysate allows toxins, electrolytes, and excess water to diffuse out of the blood and into the dialysate.
Step 4: Dialysate Preparation and Disposal
Dialysate, a solution composed of water, electrolytes, and bicarbonate, absorbs waste products from the blood. Once it has absorbed these substances, the used dialysate exits the dialyzer and is discarded, replaced by fresh dialysate to continue the process.
Step 5: Blood Monitoring and Returning to the Patient
Monitors throughout the machine check blood pressure, temperature, and flow rate to maintain safety. Once filtration is complete, filtered blood is returned to the patient through the second arm of the AV access. The process typically takes 3 to 5 hours and is repeated multiple times per week.
5. Safety Mechanisms in Dialysis Machines
Dialysis machines are equipped with several safety mechanisms to prevent potential complications. These include:
- Air Detector: Prevents air from entering the bloodstream.
- Pressure Monitors: Regulate blood and dialysate pressure to prevent damage to blood vessels.
- Temperature Control: Keeps dialysate at body temperature to avoid patient discomfort.
- Conductivity Monitor: Ensures proper dialysate concentration for safe blood filtration.
6. Understanding Dialysis Machine Parameters
Healthcare providers monitor specific machine settings, including:
- Blood Flow Rate (BFR): Controls how quickly blood is filtered.
- Dialysate Flow Rate (DFR): Regulates how fast dialysate passes through the dialyzer.
- UF (Ultrafiltration) Rate: Determines how much fluid is removed from the patient.
- Dialysate Temperature and Conductivity: Ensures dialysate is safe and effective for filtration.
7. Maintenance and Troubleshooting
Routine maintenance of dialysis machines is essential to prevent breakdowns and ensure patient safety. This involves regularly cleaning and disinfecting the machine, checking filters, and calibrating sensors. Staff are trained to troubleshoot common alarms and monitor machine performance throughout each session.
8. Benefits of Dialysis Machines in Healthcare
Dialysis machines play an invaluable role in healthcare by:
- Supporting patients with end-stage renal disease (ESRD) or acute kidney injury.
- Helping stabilize patients’ fluid, electrolyte, and pH levels.
- Offering life-extending treatment options, often bridging the gap until kidney transplantation.
Conclusion
Dialysis machines are intricate yet lifesaving devices essential for patients with severe kidney impairment. By understanding the working process and safety mechanisms of dialysis machines, healthcare providers and patients alike can better appreciate the vital role they play in managing renal health. Regular advancements in dialysis technology continue to improve patient outcomes, making dialysis safer, more efficient, and increasingly comfortable.










Leave a Reply