Preventing Ventilator-Associated Pneumonia (VAP) in the ICU: Best Practices
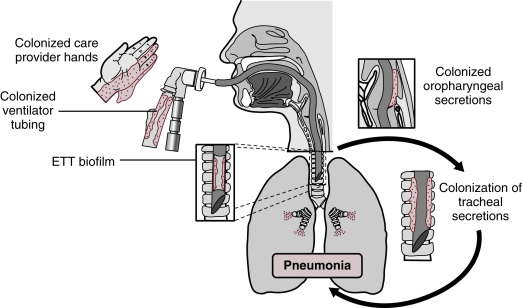
Ventilator-associated pneumonia (VAP) is a significant concern in Intensive Care Units (ICUs), contributing to longer hospital stays, increased medical costs, and a higher risk of mortality. VAP occurs when patients on mechanical ventilation develop lung infections, usually 48 hours after intubation. Fortunately, various best practices can significantly reduce the occurrence of VAP, protecting vulnerable patients and improving outcomes. Here’s a comprehensive look at key strategies for preventing VAP in the ICU.
1. Implement a VAP Bundle Approach
A “VAP bundle” consists of a set of evidence-based practices applied consistently to prevent ventilator-associated pneumonia. The key components typically include:
- Elevating the Head of the Bed: Raising the head of the bed between 30-45 degrees reduces the risk of aspiration, a major cause of VAP.
- Daily Sedation Interruption: Also known as “sedation vacations,” this practice helps assess the patient’s readiness for extubation, reducing unnecessary ventilation days.
- Peptic Ulcer Prophylaxis: To prevent stress ulcers, reducing stomach acidity can help lower the risk of bacterial colonization and subsequent aspiration into the lungs.
- Deep Vein Thrombosis (DVT) Prophylaxis: Preventing blood clots helps maintain overall patient health and mobility, reducing VAP risk.
- Daily Oral Care with Chlorhexidine: Regular oral care significantly reduces the bacterial load in the mouth, lowering the chances of respiratory infections.
Studies have shown that hospitals applying the full VAP bundle can dramatically reduce the incidence of VAP and improve patient outcomes.
2. Maintain Proper Oral Hygiene
Oral hygiene is a critical, yet sometimes overlooked, aspect of VAP prevention. Bacteria from the mouth and throat can easily enter the lungs, especially in intubated patients. Regular oral care, typically with chlorhexidine mouthwash, helps to keep bacterial colonies under control.
- Chlorhexidine Mouthwash: This antiseptic solution reduces the bacterial count in the mouth, preventing bacterial migration into the respiratory system.
- Oral Suctioning: Regular suctioning of secretions helps to prevent the pooling of fluids that can harbor bacteria.
3. Minimize Ventilation Duration
The longer a patient remains on mechanical ventilation, the higher their risk of developing VAP. For this reason, minimizing the duration of ventilation is one of the most effective preventive measures.
- Early Extubation: Regular assessments for readiness to extubate can help reduce ventilation time. This includes daily interruption of sedation and spontaneous breathing trials to determine whether the patient can breathe independently.
- Non-Invasive Ventilation (NIV): For appropriate candidates, non-invasive ventilation can be used to avoid the need for intubation entirely. NIV has been shown to reduce the risk of VAP by eliminating the exposure of the airway to external pathogens.
4. Sterile Equipment and Proper Hand Hygiene
Maintaining a sterile environment is essential in reducing VAP. Healthcare workers should be vigilant about:
- Hand Hygiene: Regular hand washing with soap or alcohol-based hand sanitizers before and after patient contact, handling ventilators, or performing any invasive procedures is critical in preventing the spread of infection.
- Sterile Ventilator Equipment: Proper cleaning and disinfection of ventilator circuits and associated equipment, as well as the use of disposable or sterilized tubes, can reduce the risk of introducing infections.
- Closed Suctioning Systems: Closed suction systems reduce the risk of contaminating the patient’s airway during secretion removal and prevent the introduction of pathogens.
5. Optimizing Ventilator Settings and Humidification
Careful management of the ventilator itself can reduce VAP risk. Best practices include:
- Optimal Humidification: The use of heated humidifiers or heat-and-moisture exchangers (HMEs) prevents the drying of the airways and reduces the risk of airway injury and infection.
- Proper Cuff Pressure Management: Ensuring that the endotracheal tube cuff is adequately inflated can prevent secretions from pooling around the tube and entering the lungs.
- Subglottic Secretion Drainage: Specialized endotracheal tubes that allow for drainage of secretions above the cuff can prevent secretions from entering the lungs and causing infection.
6. Antibiotic Stewardship
Although antibiotics are often used to treat infections, overuse can lead to antibiotic resistance, making it harder to treat VAP when it occurs. Implementing an antibiotic stewardship program ensures that antibiotics are used appropriately and only when necessary. This involves:
- Culturing Respiratory Secretions: Before starting antibiotics, respiratory secretions should be cultured to identify the specific bacteria involved.
- De-escalation: Once the bacterial pathogen is identified, broad-spectrum antibiotics should be narrowed to target the specific infection, reducing the risk of resistance development.
7. Proper Use of Prophylactic Measures
Certain preventive measures, such as the use of peptic ulcer prophylaxis and thromboprophylaxis, are important components of the VAP bundle. However, these interventions should be carefully managed based on individual patient risk factors to avoid adverse effects, like increased gastric acidity leading to infection.
Conclusion
Preventing VAP in the ICU requires a multidisciplinary approach, with consistent application of best practices. From oral care and maintaining a sterile environment to minimizing ventilation duration and optimizing ventilator settings, each step plays a crucial role in reducing the risk of VAP and improving patient outcomes. Hospitals that adhere to these guidelines not only help safeguard their patients but also reduce the length of ICU stays, cut healthcare costs, and enhance overall patient recovery.
By following these evidence-based best practices, ICU teams can make a significant impact in reducing the incidence of ventilator-associated pneumonia, ultimately saving lives and improving the quality of care for critically ill patients.









Leave a Reply