Non-Invasive Ventilation and Its Effect on Reducing Ventilator-Associated Pneumonia (VAP)
Introduction
Ventilator-Associated Pneumonia (VAP) is a major concern in Intensive Care Units (ICUs), especially for patients on mechanical ventilation. VAP is linked to increased hospital stays, higher costs, and greater mortality rates. Non-Invasive Ventilation (NIV) offers an effective alternative to traditional invasive mechanical ventilation, providing respiratory support without the need for intubation. This technique has shown promise in reducing the risk of VAP and improving patient outcomes.
What is Non-Invasive Ventilation (NIV)?
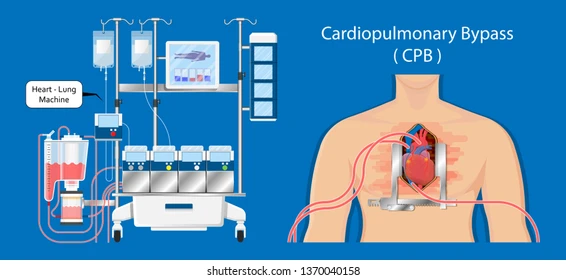
Non-Invasive Ventilation involves providing ventilatory support to patients using a mask or similar interface rather than invasive methods like endotracheal tubes. Commonly used in conditions such as Chronic Obstructive Pulmonary Disease (COPD), heart failure, and acute respiratory failure, NIV maintains oxygenation and ventilation while keeping the patient’s airway intact.
The two main types of NIV include:
- Continuous Positive Airway Pressure (CPAP): Maintains constant air pressure to keep the airways open.
- Bi-Level Positive Airway Pressure (BiPAP): Provides variable air pressure, delivering higher pressure during inhalation and lower pressure during exhalation.
How NIV Helps Reduce Ventilator-Associated Pneumonia
- Avoids Intubation One of the key reasons why NIV reduces VAP risk is that it eliminates the need for intubation. Endotracheal tubes create a direct pathway for pathogens to enter the lungs, increasing the risk of infection. By bypassing this route, NIV minimizes the chance of bacteria entering the respiratory system, which is crucial in preventing VAP.
- Preserves Natural Airway Defenses Intubation compromises the natural defenses of the upper respiratory tract, such as coughing and mucociliary clearance. NIV allows patients to retain these defense mechanisms, reducing the chance of colonization by harmful bacteria that can lead to pneumonia.
- Shorter Duration of Ventilatory Support Studies have shown that patients on NIV often require shorter periods of ventilatory support compared to those on invasive ventilation. This reduced duration lowers the cumulative exposure to potential infections, decreasing the likelihood of developing VAP.
- Improved Patient Comfort and Cooperation NIV is generally more comfortable for patients, leading to better compliance and cooperation. When patients are more cooperative, it becomes easier to maintain effective lung expansion and avoid complications such as atelectasis (lung collapse), which is a risk factor for pneumonia.
- Reduced Sedation Requirements Patients on invasive ventilation often need heavy sedation to tolerate the discomfort of intubation. Sedation, however, can suppress immune responses and impair mobility, both of which increase the risk of pneumonia. NIV reduces the need for sedation, allowing patients to remain more alert and mobile, further decreasing their risk of infection.
Evidence Supporting NIV in Reducing VAP Risk
Several clinical studies have demonstrated the effectiveness of NIV in reducing the incidence of VAP. For instance, a meta-analysis of randomized controlled trials found that patients on NIV had a significantly lower risk of VAP compared to those on invasive ventilation. Another study revealed that NIV can reduce VAP incidence by up to 60%, particularly in patients with acute respiratory failure.
In addition to reducing VAP, NIV has also been linked to shorter hospital stays, lower healthcare costs, and decreased mortality rates, making it a valuable tool in ICU care.
When is NIV Appropriate?
While NIV offers numerous benefits, it is not suitable for all patients. It is most effective in cases of mild to moderate respiratory failure where the patient can breathe spontaneously. However, it may not be appropriate for patients with severe hypoxemia, altered mental status, or other conditions requiring full mechanical ventilation.
Challenges in Using NIV
Despite its advantages, there are some challenges in implementing NIV:
- Mask Discomfort: Some patients find wearing the mask uncomfortable, which can lead to poor compliance.
- Air Leaks: Improperly fitted masks can cause air leaks, reducing the effectiveness of ventilation.
- Aspiration Risk: NIV can increase the risk of aspiration in some patients, especially if used inappropriately or if the patient is unable to protect their airway.
Conclusion
Non-Invasive Ventilation is a powerful tool in reducing the risk of Ventilator-Associated Pneumonia. By avoiding intubation, preserving natural airway defenses, and minimizing sedation requirements, NIV provides a safer alternative for many patients needing respiratory support. Although it may not be suitable for all clinical situations, when used appropriately, NIV can significantly improve outcomes, decrease VAP rates, and reduce the overall burden of care in the ICU.
As the use of NIV continues to expand, healthcare professionals must be well-versed in its application and management to maximize its benefits and minimize potential complications.










Leave a Reply