The Impact of Health Policy on Hospital Management: A Guide for Healthcare Administrators
Hospitals are complex organisations that depend heavily on public health policies to ensure smooth operations, high-quality patient care, and financial sustainability. Healthcare administrators play a critical role in adapting to these policies, which shape everything from workforce management to budget allocation and patient safety protocols. This blog will explore how health policy affects hospital management and provide strategies for administrators to navigate these challenges successfully.
1. Understanding the Role of Health Policy in Hospitals
Health policies—whether enacted at the federal, state, or local levels—serve as a foundation for the management of hospitals and healthcare institutions. These policies regulate important aspects like quality of care, access to services, cost control, and patient safety. Healthcare administrators must stay updated on policy changes to ensure that their hospital complies with regulations, such as staffing requirements, infection control measures, or billing and reimbursement guidelines.
One of the most impactful policies in recent years is the Affordable Care Act (ACA), which dramatically changed how hospitals handle patient care and insurance billing. The ACA introduced mandatory quality reporting and value-based reimbursement, linking hospital performance directly to financial incentives. This means that healthcare administrators must now focus on both the quality of care and the operational efficiency of their institutions to maximize revenue.
2. Budgeting and Resource Allocation
Health policy affects hospital budgeting and resource allocation in profound ways. Policies related to reimbursement (like those from Medicare and Medicaid) impact how hospitals are paid for the care they provide. Administrators must plan hospital budgets to account for these payment systems and adjust for changes, such as reductions in reimbursements for certain services.
The introduction of value-based care, where hospitals are paid based on patient outcomes rather than the number of services provided, has forced administrators to re-evaluate resource allocation. Hospitals must now invest more in technology, staff training, and preventive care programs to improve outcomes and maintain financial stability.
3. Workforce Management and Staffing
Health policies also directly influence how hospitals manage their workforce. Regulations set by bodies like the Joint Commission or the Centers for Medicare & Medicaid Services (CMS) mandate minimum staffing levels, licensure requirements, and ongoing professional development. For example, policies may dictate nurse-to-patient ratios in certain hospital departments, affecting staffing decisions and budget allocations.
Healthcare administrators must ensure that their hospitals comply with these staffing requirements while managing labor costs. This includes balancing full-time staff with contract workers and making sure the hospital is equipped to handle workforce shortages, particularly during public health emergencies like the COVID-19 pandemic.
4. Quality and Patient Safety
Public health policies are designed to enhance patient safety and quality of care. Programs like the Hospital Readmissions Reduction Program (HRRP) penalize hospitals with high readmission rates, incentivizing them to improve post-discharge care and follow-up. In addition, policies from the Centers for Disease Control and Prevention (CDC) regarding infection control shape how hospitals design protocols to prevent hospital-acquired infections (HAIs).
Healthcare administrators are responsible for implementing these policies and ensuring that all hospital staff adhere to them. This includes investing in the necessary tools and technologies to monitor compliance, such as electronic health records (EHR) systems and infection tracking software.
5. Adapting to Policy Changes: A Strategic Approach
As health policies continue to evolve, healthcare administrators must remain agile. Key strategies include:
- Continuous Education: Administrators should stay informed about upcoming regulatory changes and policy updates. This can be achieved through regular training and by maintaining strong relationships with legal and compliance teams.
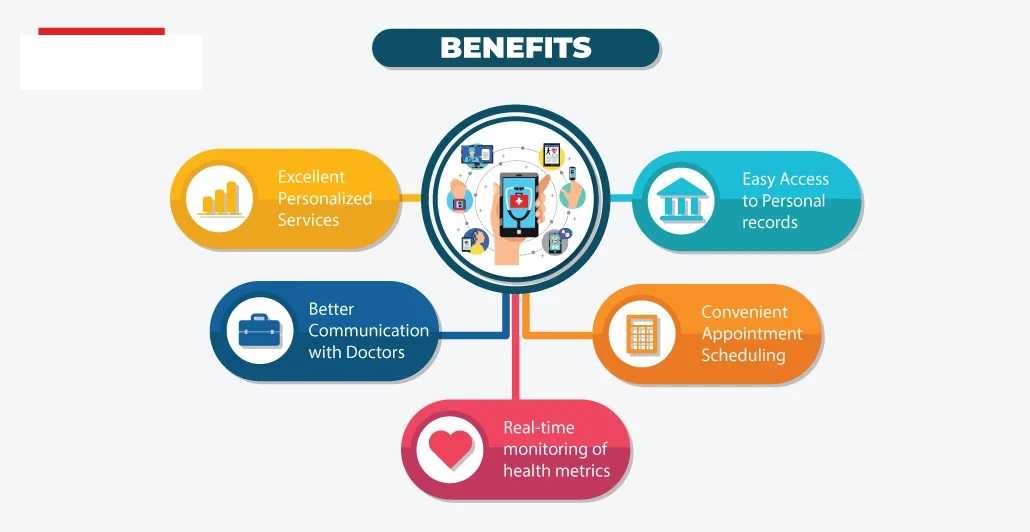
- Technology Investments: With policies pushing for more digital integration, hospitals must invest in technologies like telemedicine, EHR systems, and health information exchanges (HIE) to stay compliant and improve patient care.
- Data-Driven Decision Making: Leveraging data analytics can help administrators understand the impact of health policies on their hospital’s performance. This insight allows them to make informed decisions regarding staffing, resource allocation, and quality improvement.
- Collaboration and Advocacy: Hospital leaders should work with policymakers to advocate for regulations that benefit their institution and community. This might include engaging in discussions with health policy boards or being active in healthcare advocacy groups.
Conclusion
Health policies shape every aspect of hospital management, from budgeting to patient care. For healthcare administrators, understanding and adapting to these policies is crucial for ensuring operational efficiency, financial stability, and high-quality patient care. By staying informed and proactive, administrators can successfully navigate the challenges posed by evolving healthcare regulations and create a more resilient, efficient healthcare system.









Leave a Reply