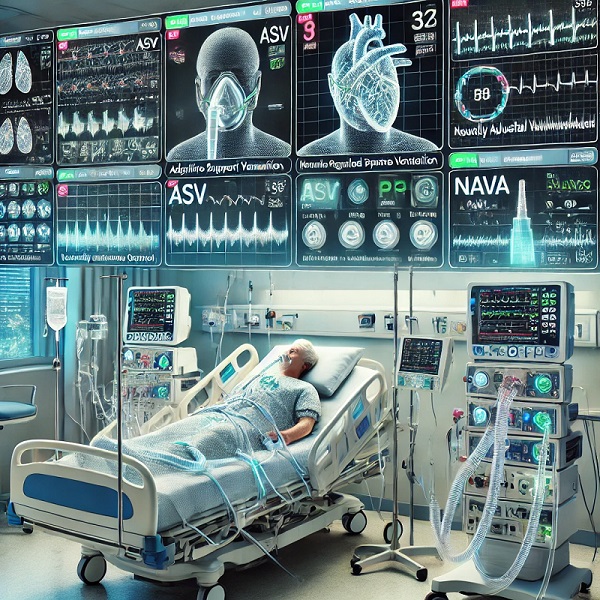
Understanding Adaptive Ventilation Modes in ICU: A Guide to ASV, PRVC, and NAVA
Mechanical ventilation is a lifesaving intervention in critical care like ICU, and advancements in ventilator technology have led to the development of adaptive ventilation modes that tailor support based on the patient’s respiratory mechanics. Three key adaptive modes used in the ICU are Adaptive Support Ventilation (ASV), Pressure-Regulated Volume Control (PRVC), and Neurally Adjusted Ventilatory Assist (NAVA). These modes adaptive ventilation modes not only optimise patient comfort but also gas exchange and reduce the risks of ventilator-induced lung injury (VILI).
Let’s explore each mode in detail.

1. Adaptive Support Ventilation (ASV)
What It Is:
ASV is an advanced, closed-loop mode of ventilation that continuously monitors the patient’s respiratory parameters—such as tidal volume, respiratory rate, and lung compliance—and automatically adjusts the level of support. This mode works to maintain an optimal level of ventilation based on the patient’s needs, whether they are completely reliant on the ventilator or partially breathing on their own.
How It Works:
ASV adjusts the inspiratory pressure, breath frequency, and tidal volume based on feedback from the patient’s respiratory mechanics. It is particularly effective for patients with rapidly changing conditions, such as those recovering from acute respiratory failure, as it reduces the need for frequent manual adjustments by the healthcare provider.
Advantages:
- Automatically adapts to the patient’s lung condition.
- Reduces the likelihood of over- or under-ventilation.
- Improves patient-ventilator synchrony, enhancing comfort and recovery
Clinical Application:
ASV is commonly used in post-operative patients and those transitioning from full ventilation to spontaneous breathing. By automatically adjusting support, it helps in weaning patients off the ventilator, minimizing risks of prolonged mechanical ventilation.
2. Pressure-Regulated Volume Control (PRVC)
What It Is:
PRVC is a dual-controlled ventilation mode that combines the benefits of both pressure-controlled and volume-controlled ventilation. In this mode, the ventilator delivers a preset tidal volume while adjusting the pressure to achieve this target based on the patient’s lung compliance and resistance.
How It Works:
The ventilator monitors each breath and adjusts the inspiratory pressure to ensure the desired tidal volume is delivered with the least amount of pressure. If the patient’s lung compliance worsens (for instance, due to fluid overload or infection), the ventilator increases the pressure to maintain the tidal volume.
Advantages:
- Ensures consistent tidal volume delivery while minimizing the risk of barotrauma (pressure-related lung injury).
- Reduces the variability in gas exchange, providing reliable oxygenation and CO2 elimination.
- Ideal for patients with fluctuating lung conditions, such as Acute Respiratory Distress Syndrome (ARDS)
PRVC is especially useful in patients with conditions like ARDS, where maintaining lung protection is crucial. It’s also widely used in pediatric and neonatal care, where gentle and controlled ventilation is needed.
3. Neurally Adjusted Ventilatory Assist (NAVA)
What It Is:
NAVA represents a significant advancement in patient-ventilator interaction by using the electrical activity of the diaphragm (EAdi) to guide ventilation. In this mode, a special catheter placed in the esophagus detects diaphragm signals, and the ventilator delivers assistance proportional to the patient’s effort.
How It Works:
When the diaphragm contracts, the ventilator senses the electrical activity and provides pressure support in sync with the patient’s own breathing efforts. This ensures natural breathing patterns and minimizes the risk of ventilator-induced lung injury.
Advantages:
- Highly precise patient-ventilator synchrony.
- Reduced risk of over-assistance and under-assistance.
- Improves comfort and is particularly useful in weaning patients off mechanical ventilation(
Clinical Application:
NAVA is especially beneficial for patients with complex respiratory needs, such as those with neuromuscular disorders or irregular breathing patterns. It is also effective during the weaning phase, allowing for a more gradual transition from ventilator dependence.
Why These Adaptive Modes Matter in the ICU
Adaptive ventilator modes like ASV, PRVC, and NAVA provide individualized respiratory support that responds to the patient’s needs in real time. This personalized approach improves patient outcomes by reducing complications such as barotrauma, volutrauma, and ventilator-associated pneumonia (VAP). These modes are also integral in enhancing patient comfort and improving the success rate of weaning from mechanical ventilation.
Benefits of Adaptive Modes:
- Improved patient safety by preventing over-ventilation.
- Enhanced patient-ventilator synchrony reduces discomfort.
- Greater flexibility in managing patients with varying respiratory mechanics.
In conclusion, the integration of adaptive modes into ICU care has revolutionized mechanical ventilation. Understanding how these modes function helps clinicians tailor respiratory support to optimize patient outcomes, reduce complications, and facilitate quicker recovery.










वेंटिलेटर मोड्स: उपयोग, प्रकार और स्वास्थ्य लाभ - My Blog
[…] Read this……… […]